Rural Health in Connecticut (2022)
A comprehensive review of social determinants, community resources, health outcomes, and wellbeing

Introduction (excerpt)
This 2022 report is an update and expansion upon “An Assessment of Rural Health in Connecticut: Overview, Obstacles, and Opportunities” — the previous rural health assessment completed in 2015.
Public health data and ways of reporting that data have changed since the completion of the 2015 report. More datasets are now publicly available with estimates of health related indicators at a variety of geographic levels. Public health emphasis has also shifted to accommodate a better understanding of the social determinants that influence healthy behavior and help prevent major illnesses. With more detailed data, we can now disaggregate information by race/ethnicity, sex, and other demographic factors. As a result, public health reporting has seen a renewed focus on social and health equity.
Specific trends in health outcomes have also become more apparent. The alarming rise of fentanyl in the illicit drug supply has led to steep increases in drug related fatalities, and the opioid epidemic has been recognized as being multifaceted—affecting rural and urban populations differently. Finally, the COVID-19 pandemic has been one of the most turbulent public health crises in a lifetime, upending social and economic foundations that influence overall health and wellbeing, exposing deep inequities in health care quality and access, and testing the resilience of the health care sector.
This report documents the nature of public health for Connecticut’s rural populations with a renewed focus on trends to better capture how these populations are changing. Disaggregations by race/ethnicity and age are used to better understand the health needs of different populations.
Also, notably, this report shifts away from geographical groupings of rural towns in favor of demographic groupings of towns to better describe the ways that social determinants of health vary across populations, and affect health behaviors and outcomes.
Executive Summary (excerpt)
GROUPING RURAL TOWNS
- Three distinct groups of rural towns were revealed, based on resident age, educational attainment, and income.
- Type One Towns have fewer adults with post-secondary education and lower median household incomes compared to the other rural towns.
- Type Two Towns have higher than average shares of residents age 65 and over compared to the other rural towns.
- Type Three Towns have very high median household incomes and are usually closer in proximity to Connecticut’s larger cities.
DEMOGRAPHICS & SOCIAL DETERMINANTS OF HEALTH
- Population in rural towns has declined slightly between 2010 and 2020.
- Younger generations are more racially and ethnically diverse.
- There are rising shares of high-needs students in public schools, suggesting that educational and social services resources for children are as important as ever.
- Income disparities like poverty, financial insecurity, and food insecurity are not evenly distributed across the population. Due to the legacy of racial discrimination in employment, housing, and education, Black, Latino, and Native American populations are more likely to experience these challenges. These populations are more prevalent in Type One Towns.
HEALTHCARE SYSTEM ASSETS & RESOURCES
- Residents of rural towns in Connecticut face longer drive times to health care facilities than the state average.
- In rural counties, there are fewer primary care providers and dentists per person compared to the state’s more urban counties.
- According to HRSA, Type One Towns have Primary Care and Dental Health Health Provider Shortage Areas, while Type Two and Type Three Towns do not.
- Workforce projections for Connecticut show that Family Practice doctors are in high demand and short supply, which may negatively affect children’s health care access.
HEALTH RISKS & BEHAVIORS
- Low-income adults and people of color are more likely to lack a person or place they consider their doctor, and are also more likely to have skipped or delayed necessary medical care.
- About 30 percent of adults statewide and in rural areas have a BMI that qualifies them as obese. Obesity is related to many other health issues such as diabetes, stroke, high blood pressure, and high cholesterol.
- Adults in Type One Towns are more likely to engage in risky health behaviors, such as binge drinking and smoking. These behaviors are related to higher rates of financial insecurity, which is elevated higher in Type One Towns.
- Adults in Type One Towns also have higher rates of hospital encounters compared to adults statewide and in other rural areas.
HEALTH OUTCOMES
- Type Two Towns, with higher shares of adults over age 65, have elevated rates of chronic health issues.
- Type One and Type Two Towns have higher shares of children with elevated blood-lead levels.
- Rural towns in general have about 3 times the rate of people diagnosed with Lyme disease.
- Non-rural towns have higher rates of death due to COVID-19 than rural towns, although Type One Towns trend close to non-rural rates.
- Rural areas generally have more positive birth outcomes than the state average, but these should be monitored closely as labor and delivery wards in rural hospitals are closed.
- Drug-related fatalities continue to increase year over year. Fentanyl is a major driver in the rise in overdose deaths, statewide and in Type One Towns.
- Despite average life expectancies in rural towns that track close with the state average. As of 2015, wide gaps within rural clusters are apparent.
- COVID-19 caused a jump in all-cause mortality in 2020, but cancer and heart disease remain the top causes of death.
- Annually, Type One Towns have higher premature death rates the state average.
Click the link at the top of the page to download the full report.
Related Reports
Related Data
Document
Disability in Connecticut: Insights from the DataHaven Community Wellbeing Survey (PDF)
Dataset, Document
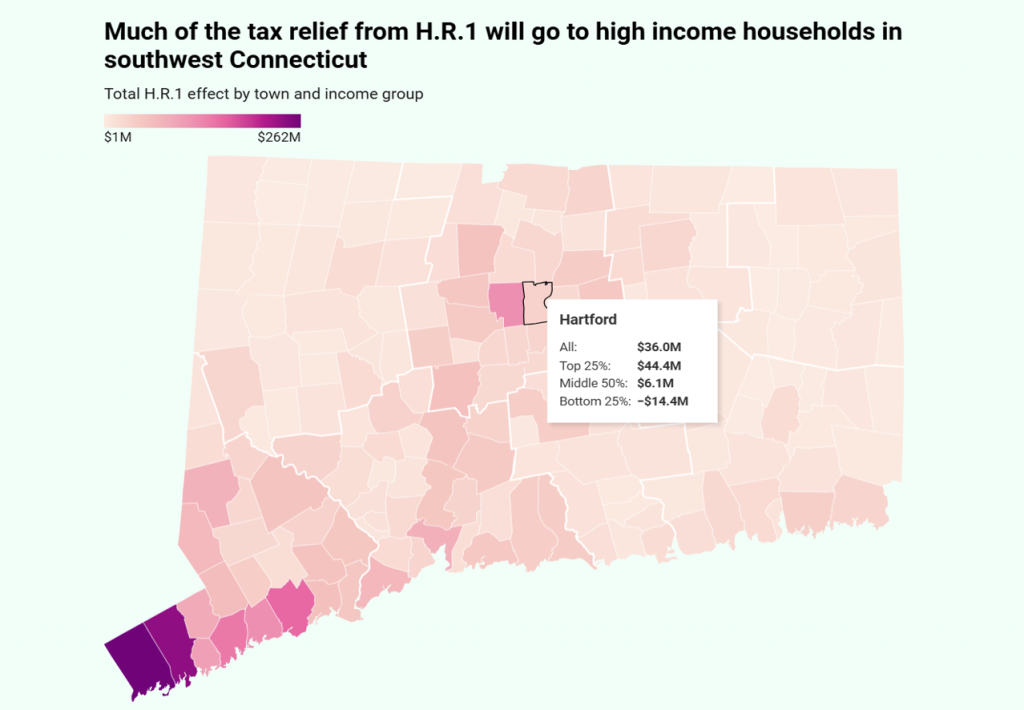
DataHaven HR1 Tax Effects Spreadsheet by Connecticut Town
Document
Wilton Town Equity Report 2025
Document
Winchester Town Equity Report 2025
Document
Windham Town Equity Report 2025
Document